Breast Cancer Symptoms and Treatment, occurs when changes called mutations take place in genes that regulate cell growth. The mutations let the cells divide and multiply in an uncontrolled way. Breast cancer is cancer that develops in breast cells. Typically, the cancer forms in either the lobules or the ducts of the breast. Lobules are the glands that produce milk, and ducts are the pathways that bring the milk from the glands to the nipple. Cancer can also occur in the fatty tissue or the fibrous connective tissue within your breast. The uncontrolled cancer cells often invade other healthy breast tissue and can travel to the lymph nodes under the arms. Once the cancer enters the lymph nodes, it has access to a pathway to move to other parts of the body. See pictures and learn more about the structure of the breast.
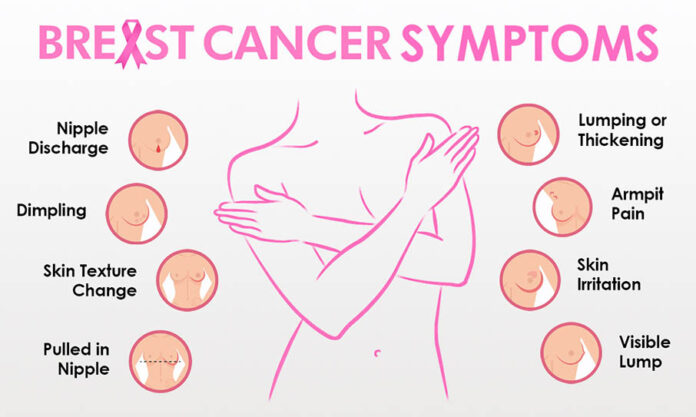
Signs and symptoms of breast cancer
In its early stages, breast cancer may not cause any symptoms. In many cases, a tumor may be too small to be felt, but an abnormality can still be seen on a mammogram.
If a tumor can be felt, the first sign is usually a new lump in the breast that was not there before. However, not all lumps are cancer.
Each type of breast cancer can cause a variety of symptoms. Many of these symptoms are similar, but some can be different. Symptoms for the most common breast cancers include:
- a breast lump or tissue thickening that feels different from surrounding tissue and is new
- breast pain
- red or discolored, pitted skin on the breast
- swelling in all or part of your breast
- a nipple discharge other than breast milk
- bloody discharge from your nipple
- peeling, scaling, or flaking of skin on your nipple or breast
- a sudden, unexplained change in the shape or size of your breast
- inverted nipple
- changes to the appearance of the skin on your breasts
- a lump or swelling under your arm
If you have any of these symptoms, it doesn’t necessarily mean you have breast cancer. For instance, pain in your breast or a breast lump can be caused by a benign cyst.
Still, if you find a lump in your breast or have other symptoms, contact your doctor for further examination and testing.
Types of breast cancer
There are several types of breast cancer, and they’re broken into two main categories: invasive and noninvasive. Noninvasive breast cancer is also known as breast cancer in situ.
While invasive cancer has spread from the breast ducts or glands to other parts of the breast, noninvasive cancer has not spread from the original tissue.
These two categories are used to describe the most common types of breast cancer, which include:
- Ductal carcinoma in situ. Ductal carcinoma in situ (DCIS) is a noninvasive condition. With DCIS, the cancer cells are confined to the ducts in your breast and haven’t invaded the surrounding breast tissue.
- Lobular carcinoma in situ. Lobular carcinoma in situ (LCIS) is cancer that grows in the milk-producing glands of your breast. Like DCIS, the cancer cells haven’t invaded the surrounding tissue.
- Invasive ductal carcinoma. Invasive ductal carcinoma (IDC) is the most common type of breast cancer. This type of breast cancer begins in your breast’s milk ducts and then invades nearby tissue in the breast. Once the breast cancer has spread to the tissue outside your milk ducts, it can begin to spread to other nearby organs and tissue.
- Invasive lobular carcinoma. Invasive lobular carcinoma (ILC) first develops in your breast’s lobules and has invaded nearby tissue.
Other, less common types of breast cancer include:
- Paget disease of the nipple. This type of breast cancer begins in the ducts of the nipple, but as it grows, it begins to affect the skin and areola of the nipple.
- Phyllodes tumor. This very rare type of breast cancer grows in the connective tissue of the breast. Most of these tumors are benign, but some are cancerous.
- Angiosarcoma. This is cancer that grows on the blood vessels or lymph vessels in the breast.
The type of cancer you have helps guide your treatment options and long-term outcome.
Inflammatory breast cancer
Inflammatory breast cancer (IBC) is a rare but aggressive type of breast cancer. According to the National Cancer Institute (NCI), IBC makes up only 1 to 5 percentTrusted Source of all breast cancer cases.
With this condition, cells block the lymph nodes near the breasts, so the lymph vessels in the breast can’t properly drain. Instead of creating a tumor, IBC causes your breast to swell, look red, and feel very warm. Your breast may appear pitted and thick, like an orange peel.
IBC can be very aggressive and can progress quickly. For this reason, it’s important to contact your doctor right away if you notice any symptoms.
Triple-negative breast cancer
Triple-negative breast cancer is another rare disease type. It affects only about 10 to 15 percentTrusted Source of people with breast cancer, according to the American Cancer Society (ACS).
To be diagnosed as triple-negative breast cancer, a tumor must have all three of the following characteristics:
- It lacks estrogen receptors. These are receptors on the cells that bind, or attach, to the hormone estrogen. If a tumor has estrogen receptors, estrogen can stimulate the cancer to grow.
- It lacks progesterone receptors. These receptors are cells that bind to the hormone progesterone. If a tumor has progesterone receptors, progesterone can stimulate the cancer to grow.
- It doesn’t have additional human epidermal growth factor receptor 2 (HER2) proteins on its surface. HER2 is a protein that fuels breast cancer growth.
If a tumor meets these three criteria, it’s labeled triple-negative breast cancer. This type of breast cancer tends to grow and spread more quickly than other types of breast cancer.
Triple-negative breast cancers are difficult to treat because hormonal therapy for breast cancer is not effective.
Breast cancer stages
Doctors divide breast cancer into stages based on the size of the tumor and how much it has spread.
Cancers that are large or have invaded nearby tissues or organs are at a higher stage than cancers that are small or still contained in the breast. To stage breast cancer, doctors need to know:
- if the cancer is invasive or noninvasive
- how large the tumor is
- whether the lymph nodes are involved
- if the cancer has spread to nearby tissue or organs
Breast cancer has five main stages: stages 0 to 4.
Stage 0 breast cancer
Stage 0 is DCIS. Cancer cells in DCIS remain confined to the ducts in the breast and have not spread into nearby tissue.
Stage 1 breast cancer
- Stage 1A. The primary tumor is 2 centimeters (cm) wide or less. The lymph nodes are not affected.
- Stage 1B. Cancer is found in nearby lymph nodes. Either there is no tumor in the breast, or the tumor is smaller than 2 cm.
Stage 2 breast cancer
- Stage 2A. The tumor is smaller than 2 cm and has spread to 1 to 3 nearby lymph nodes, or it’s between 2 and 5 cm and hasn’t spread to any lymph nodes.
- Stage 2B. The tumor is between 2 and 5 cm and has spread to 1 to 3 axillary (armpit) lymph nodes, or it’s larger than 5 cm and hasn’t spread to any lymph nodes.
Stage 3 breast cancer
- Stage 3A.
- The cancer has spread to 4 to 9 axillary lymph nodes or has enlarged the internal mammary lymph nodes. The primary tumor can be any size.
- Tumors are greater than 5 cm. The cancer has spread to 1 to 3 axillary lymph nodes or any breastbone nodes.
- Stage 3B. A tumor has invaded the chest wall or skin and may or may not have invaded up to 9 lymph nodes.
- Stage 3C. Cancer is found in 10 or more axillary lymph nodes, lymph nodes near the collarbone, or internal mammary nodes.
Stage 4 breast cancer (metastatic breast cancer)
Stage 4 breast cancer can have a tumor of any size. Its cancer cells have spread to nearby and distant lymph nodes as well as distant organs.
The testing your doctor does will determine the stage of your breast cancer, which will affect your treatment.
Male breast cancer
Although they generally have less of it, men have breast tissue just like women do. Men can develop breast cancer too, but it’s much rarer.
According to the ACSTrusted Source, breast cancer is 70 times less common in Black men than in Black women. It’s 100 times less common in white men than in white women.
That said, the breast cancer that men develop is just as serious as the breast cancer that women develop. It also has the same symptoms. If you’re a man, follow the same monitoring instructions as women and report any changes to breast tissue or new lumps to your doctor.
Breast cancer survival rate
Breast cancer survival rates vary widely based on many factors.
Two of the most important factors are the type of cancer you have and the stage of the cancer at the time you receive a diagnosis. Other factors that may play a role include:
- your age
- your gender
- your race
- the growth rate of the cancer
Research from 2021Trusted Source shows there’s a higher mortality rate in People of Color with breast cancer diagnoses compared with white people. One reason for this may be healthcare disparities.
The good news is breast cancer survival rates are improving.
According to the ACSTrusted Source, in 1975, the 5-year survival rate for breast cancer in women was 75.2 percent. But for women diagnosed between 2008 and 2014, it was 90.6 percent.
The 5-year survival rates for breast cancer differ depending on the stage at diagnosis. They range from 99 percent for localized early stage cancers to 27 percent for advanced metastatic cancers.
Diagnosis of breast cancer
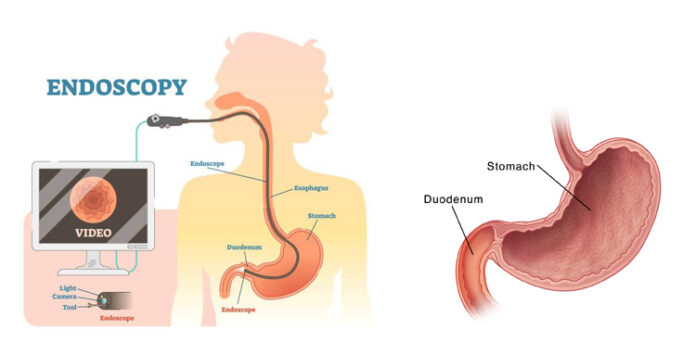
To determine if your symptoms are caused by breast cancer or a benign breast condition, your doctor will do a thorough physical exam in addition to a breast exam. They may also request one or more diagnostic tests to help understand what’s causing your symptoms.
Tests that can help your doctor diagnose breast cancer include:
- Mammogram. The most common way to see below the surface of your breast is with an imaging test called a mammogram. Many women ages 40 and older get annual mammograms to check for breast cancer. If your doctor suspects you may have a tumor or suspicious spot, they will also request a mammogram. If an atypical area is seen on your mammogram, your doctor may request additional tests.
- Ultrasound. A breast ultrasound uses sound waves to create a picture of the tissues deep in your breast. An ultrasound can help your doctor distinguish between a solid mass, such as a tumor, and a benign cyst.
Your doctor may also suggest tests such as an MRI or a breast biopsy.
If you don’t already have a primary care doctor, you can browse doctors in your area through the Healthline FindCare tool.
Breast biopsy
If your doctor suspects breast cancer based on tests like a mammogram or an ultrasound, they may do a test called a breast biopsy.
During this test, your doctor will remove a tissue sample from the suspicious area to have it tested.
There are several types of breast biopsies. With some of these tests, your doctor uses a needle to take the tissue sample. With others, they make an incision in your breast and then remove the sample.
Your doctor will send the tissue sample to a laboratory. If the sample tests positive for cancer, the lab can test it further to tell your doctor what type of cancer you have.
Breast cancer treatment
Your breast cancer’s stage, how far it has invaded (if it has), and how big the tumor has grown all play a large part in determining what kind of treatment you’ll need.
To start, your doctor will determine your cancer’s size, stage, and grade. Your cancer’s grade describes how likely it is to grow and spread. After that, you can discuss your treatment options.
Surgery is the most common treatment for breast cancer. Many people have additional treatments, such as chemotherapy, targeted therapy, radiation, or hormone therapy.
Surgery
Several types of surgery may be used to remove breast cancer, including:
- Lumpectomy. This procedure removes the tumor and some surrounding tissue, leaving the rest of the breast intact.
- Mastectomy. In this procedure, a surgeon removes an entire breast. In a double mastectomy, they remove both breasts.
- Sentinel node biopsy. This surgery removes a few of the lymph nodes that receive drainage from the tumor. These lymph nodes will be tested. If they don’t have cancer, you may not need additional surgery to remove more lymph nodes.
- Axillary lymph node dissection. If lymph nodes removed during a sentinel node biopsy contain cancer cells, your doctor may remove additional lymph nodes.
- Contralateral prophylactic mastectomy. Even though breast cancer may be present in only one breast, some people elect to have a contralateral prophylactic mastectomy. This surgery removes your healthy breast to lower your risk of developing breast cancer again.
Radiation therapy
With radiation therapy, high-powered beams of radiation are used to target and kill cancer cells. Most radiation treatments use external beam radiation. This technique uses a large machine on the outside of the body.
Advances in cancer treatment have also enabled doctors to irradiate cancer from inside the body. According to Breastcancer.org, this type of radiation treatment is called brachytherapy.
To conduct brachytherapy, surgeons place radioactive seeds, or pellets, inside the body near the tumor site. The seeds stay there for a short period of time and work to destroy cancer cells.
Chemotherapy
Chemotherapy is a drug treatment used to destroy cancer cells. Some people may undergo chemotherapy on its own, but this type of treatment is often used along with other treatments, especially surgery.
Some people will have surgery first followed by other treatments, such as chemo or radiation. This is called adjuvant therapy. Others may have chemotherapy first to shrink the cancer, called neoadjuvant therapy, then surgery.
In some cases, doctors prefer to give chemotherapy before surgery. The hope is that the treatment will shrink the tumor, and then the surgery will not need to be as invasive.
Chemotherapy has many unwanted side effects, so discuss your concerns with your doctor before starting treatment.
Hormone therapy
If your type of breast cancer is sensitive to hormones, your doctor may start you on hormone therapy. Estrogen and progesterone, two female hormones, can stimulate the growth of breast cancer tumors.
Hormone therapy works by blocking your body’s production of these hormones or by blocking the hormone receptors on the cancer cells. This action can help slow and possibly stop the growth of your cancer.
Additional medications
Certain treatments are designed to attack specific irregularities or mutations within cancer cells.
For example, Herceptin (trastuzumab) can block your body’s production of the HER2 protein. HER2 helps breast cancer cells grow, so taking a medication to slow the production of this protein may help slow cancer growth.
Your doctor will tell you more about any specific treatment they recommend for you.
Breast cancer pictures
Breast cancer can cause a range of symptoms, and these symptoms can appear differently in different people.
If you’re concerned about a spot or change in your breast, it can be helpful to know what breast problems that are actually cancer look like.
Breast cancer care
If you detect an unusual lump or spot in your breast or have any other symptoms of breast cancer, make an appointment to visit your doctor.
Chances are good that it’s not breast cancer. For instance, there are many other potential causes for breast lumps.
But if your problem does turn out to be cancer, keep in mind that early treatment is the key. Early stage breast cancer can often be treated and cured if found quickly enough. The longer breast cancer can grow, the more difficult treatment becomes.
If you’ve already received a breast cancer diagnosis, keep in mind that cancer treatments continue to improve, as do outcomes. So follow your treatment plan and try to stay positive.
Find out more about the outlook for different stages of breast cancer.
How common is breast cancer?
Bezzy Breast Cancer is a free app for people who have faced a breast cancer diagnosis. The app is available on the App Store and Google Play. Download here.
According to the Centers for Disease Control and Prevention (CDC)Trusted Source, breast cancer is the second most common cancer in women.
According to the ACSTrusted Source, in the United States in 2021, an estimated 281,550 new cases of invasive breast cancer were diagnosed in women, and 2,650 cases diagnosed in men. An additional 49,290 cases of DCIS were diagnosed in women. An estimated 44,130 breast cancer deaths occurred in 2021, including 43,600 women and 530 men.
Risk factors for breast cancer
There are several risk factors that increase your chances of getting breast cancer. However, having any of these doesn’t mean you will definitely develop the disease.
Some risk factors can’t be avoided, such as family history. You can change other risk factors, such as smoking. Risk factors for breast cancer include:
- Age. Your risk of developing breast cancer increases as you age. Most invasive breast cancers are found in women over 55 years old.
- Drinking alcohol. Alcohol use disorder raises your risk.
- Having dense breast tissue. Dense breast tissue makes mammograms hard to read. It also increases your risk of breast cancer.
- Gender. According to the ACSTrusted Source, white women are 100 times more likely to develop breast cancer than white men, and Black women are 70 times more likely to develop breast cancer than Black men.
- Genes. People who have the BRCA1 and BRCA2 gene mutations are more likely to develop breast cancer than people who don’t. Other gene mutations may also affect your risk.
- Early menstruation. If you had your first period before you were 12 years old, you have an increased risk of breast cancer.
- Giving birth at an older age. People who have their first child after 35 years old have an increased risk of breast cancer.
- Hormone therapy. People who took or are taking postmenopausal estrogen and progesterone medications to help reduce their signs of menopause symptoms have a higher risk of breast cancer.
- Inherited risk. If a close female relative has had breast cancer, you have an increased risk of developing it. This includes your mother, grandmother, sister, or daughter. If you don’t have a family history of breast cancer, you can still develop breast cancer. In fact, most people who develop it have no family history of the disease.
- Late menopause start. People who start menopause after they’re 55 years old are more likely to develop breast cancer.
- Never having been pregnant. People who have never become pregnant or carried a pregnancy to full term are more likely to develop breast cancer.
- Previous breast cancer. If you have had breast cancer in one breast, you have an increased risk of developing breast cancer in your other breast or in a different area of the previously affected breast.
Breast cancer prevention
While there are risk factors you can’t control, following a healthy lifestyle, getting regular screenings, and taking any preventive measures your doctor recommends can help lower your risk of developing breast cancer.
Lifestyle factors
Lifestyle factors can affect your risk of breast cancer.
For instance, people who have obesity have a higher risk of developing breast cancer. Maintaining a nutrient-dense diet and getting regular exercise as often as possible could help you lose weight and lower your risk.
According to the American Association for Cancer Research, alcohol misuse also increases your risk. This can be having more than two drinks per day or binge-drinking.
If you drink alcohol, talk with your doctor about what amount they recommend for you.
Breast cancer screening
Having regular mammograms may not prevent breast cancer, but it can help reduce the chance that it will go undetected.
The American College of Physicians (ACP) provides the following general recommendations for women at average risk of breast cancer:
- Women ages 40 to 49. An annual mammogram isn’t recommended, but discuss your preferences with your doctor.
- Women ages 50 to 74. A mammogram every other year is recommended.
- Women 75 years and older. Mammograms are no longer recommended.
The ACP also recommends against mammograms for women with a life expectancy of 10 years or less.
These are only guidelines.
Recommendations from the ACSTrusted Source differ. According to the ACS, women should:
- have the option of receiving annual screenings at 40 years old
- begin annual screenings at 45 years old
- move to screening every other year at 55 years old
Specific recommendations for mammograms are different for everyone, so talk with your doctor to see if you should get regular mammograms.
Preventive treatment
You may have an increased risk of breast cancer due to hereditary factors.
For instance, if your parent has a BRCA1 or BRCA2 gene mutation, you’re at higher risk of having it as well. This significantly raises your risk of breast cancer.
If you’re at risk for this mutation, talk with your doctor about your diagnostic and prophylactic treatment options. You may want to be tested to find out whether you have the mutation.
And if you learn that you do have it, talk with your doctor about any preemptive steps you can take to reduce your risk of developing breast cancer. These steps could include a prophylactic mastectomy, or surgical removal of a breast. You may also consider chemoprophylaxis, or taking medication, such as Tamoxifen, to potentially reduce your breast cancer risk.
In addition to mammograms, breast exams are another way to watch for signs of breast cancer.
Self-exams
Many people do a breast self-examination. It’s best to do this exam once per month, at the same time each month. The exam can help you become familiar with how your breasts usually look and feel so that you’re aware of any changes that occur.
Keep in mind, though, that the ACSTrusted Source considers these exams to be optional, because current research hasn’t shown a clear benefit of physical exams, whether performed at home or by a doctor.
Breast exam by your doctor
The same guidelines for self-exams provided above are true for breast exams done by your doctor or other healthcare professional. They won’t hurt you, and your doctor may do a breast exam during your annual visit.
If you’re having symptoms that concern you, it’s a good idea to have your doctor do a breast exam. During the exam, your doctor will check both of your breasts for abnormal spots or signs of breast cancer.
Your doctor may also check other parts of your body to see if the symptoms you’re having could be related to another condition.
Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and TreatmentBreast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment Breast Cancer Symptoms and Treatment





:max_bytes(150000):strip_icc()/symptoms-of-breast-cancer-430640--FINAL-b5271394bb174d14986eeea1c8035486.jpg)